The global pandemic has prompted facilities to examine their infection control measures at every level. We know the SARS-CoV-2 coronavirus can spread through exposure to small viral droplets or aerosols that stay in the air for minutes to hours. This is especially true in enclosed spaces with poor ventilation. As a result, air-sanitizing equipment that has shown to prevent disease transmission and to contribute to a healthier indoor environment is commanding greater attention in the marketplace.
One technology experiencing a recent explosion in interest is ultraviolet germicidal irradiation (UVGI), which uses ultraviolet (UV) energy to inactivate or “kill” viral, bacterial, and fungal organisms. The market for this nearly century-old technology is projected to grow 9.6% to US$570 million from 2020 to 2027, according to market research firm iHealthcareAnalyst.
What is upper-room disinfection?
According to the U.S. Centers for Disease Control and Prevention (CDC), UVGI fixtures produce UV-C energy, which has shorter wavelengths than its more penetrating cousins, UV-A and UV-B, and pose less risk to human health.
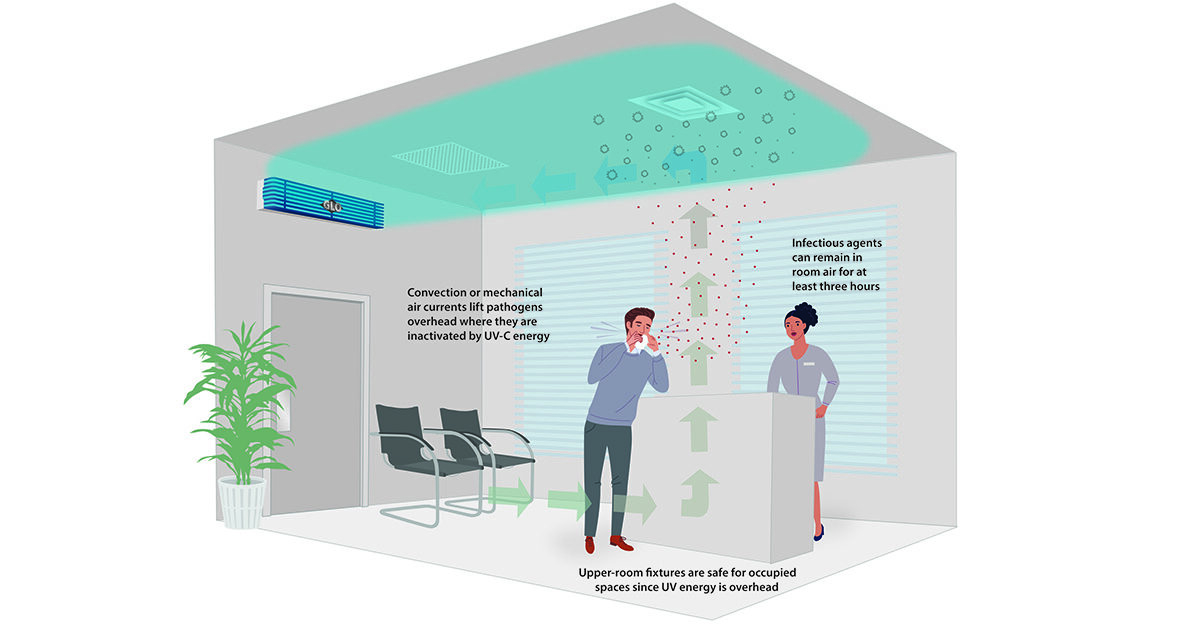
You have probably heard of UVGI, but perhaps not “upper-room UVGI,” which refers to a disinfection zone of UV energy located above people in the rooms they occupy. The UV energy inactivates airborne pathogens released in a room. Fixtures wall-mounted at a height above 7 feet prevent direct UV exposures to people in
the space.
According to Daniel Jones, president of UV Resources, a manufacturer of germicidal UV solutions, upper-room air systems are one of the oldest applications of germicidal UV for infection control. They have been used for more than 70 years to eliminate airborne pathogens, according to the CDC. “In seconds, these fixtures inactivate droplet nuclei directly at their source (from people coughing, sneezing, or talking), as well as pathogens circulated by drafts, pressure differentials, or the movement of people,” Jones explained.
How does it work?
According to the CDC, air circulated from HVAC systems, natural convection, fans, and/or open windows passes through the upper-room UVGI disinfection zone, where it receives an appropriate amount of germicidal energy. The UV energy inactivates the airborne pathogens, which can remain in the air but are no longer infectious.
Upper-room UVGI systems can also assist where existing mechanical systems cannot deliver the necessary air changes per hour. Upper room UVGI can provide multiple air change “equivalents” each hour, which helps dilute pathogen concentrations, similar to adding clean air into the space.
“Studies have shown that one hour of using an upper-room air UVC fixture can be equivalent to 10 to 16 air changes,” Jones said.
Where is it used?
In the U.S., interest in upper-room UV fixtures and airstream disinfection systems has been strongest among the health care and institutional markets (e.g., daycare centers, homeless shelters, correctional institutions), Jones noted. Approximately 60% of all UVGI air disinfection systems are installed in health care facilities, according to iHealthcareAnalyst. “However, since the pandemic struck, the biocidal qualities of UV-C have become one of the most in-demand technologies around the world, regardless of industry sector,” Jones said.
Today, you’ll often see upper-room UVGI fixtures installed in high-traffic, communal areas such as boardrooms, lunchrooms, lobbies/reception areas, lecture halls, classrooms, and in facilities such as health clubs and sport arenas.
In general, the number of upper-room UVGI fixtures required for pathogen disinfection is determined by a room’s size (germicidal coverage is specified in either square feet or cubic feet). The CDC advises that the systems be designed, installed, and tested with the help of a qualified HVAC professional or a reputable UV-system manufacturer.
What about UVGI and SARS-CoV-2?
UV research on SARS-CoV-2 indicates that the virus is very similar to other coronaviruses (e.g., SARS and MERS) regarding the UV dose necessary to inactivate it. Therefore, the CDC says upper-room UVGI systems can be a useful ventilation tool to control SARS-CoV-2 and reduce the spread of infectious pathogens.
However, the CDC clarifies that using UVGI does not replace the need for cleaning or disinfecting surfaces where infectious SARS-CoV-2 droplets may be present. In fact, infection preventionists recommend facility engineers use multilayer preventive infection-control measures to mitigate the potential spread of airborne diseases like COVID-19. In other words, UV-C alone won’t be enough. “A multibarrier approach helps ensure that whatever pathogen is not mitigated by one method (say filtering) is inactivated by another (UV-C),” Jones said.
Interest in U-VC technology won’t dwindle any time soon. Jones said due to demand, facility engineers and managers should plan for longer than traditional lead times when placing orders for UV-C systems and parts.
“Commercial demand for UV solutions is expected to remain high, as the pandemic has changed perception for the technology, shifting from a want (HVAC efficiency) to a need (health and safety),” he said.